Pharmacy
Arkansas Total Care provides high-quality and cost-effective drug therapy to our members. Arkansas Total Care covers prescription medications and some over-the-counter medications approved by providers. The pharmacy program does not cover all medications. Some medications need prior authorization, and some may have limitations.
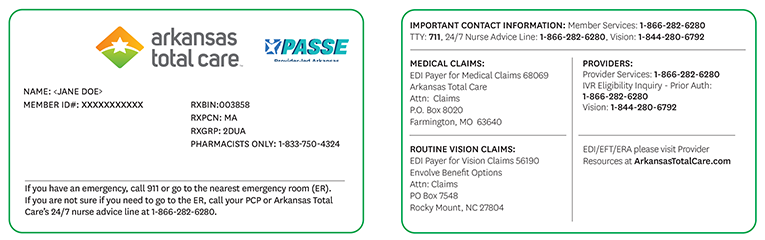
Effective January 1, 2024, Arkansas Total Care will be changing our Pharmacy Benefits Manager (PBM) to Express Scripts®. See below for new pharmacy processing information.
Pharmacy Services
For questions, please contact Pharmacy Services 24/7 at 1-833-587-2011.
Prior Authorization
Arkansas Total Care’s preferred method for submitting pharmacy prior authorization requests is through CoverMyMeds®.
CoverMyMeds is the fast and simple way to review, complete, and track prior authorization requests. Their electronic submissions process is safe, secure, and available for providers and their staff to use at no cost.
CoverMyMeds Prior Authorization Tool ›
Here are more resources if you cannot access the Pharmacy Portal:
- Arkansas Medicaid Preferred Drug List — The Preferred Drug List (PDL) (PDF) is the list of drugs covered by Arkansas Total Care. We work with providers and pharmacists to create this list. Our goal is to ensure the pharmacy benefit covers prescription medications. These medications are for a variety of conditions and diseases. The PDL applies to drugs you get at retail pharmacies. Please direct all overrides to the Pharmacy Help Desk: 1-833-750-4324 (Rx BIN: 003858).
- Healthcare Providers | Express Scripts
- Prior Authorization Request Form for Prescription Drugs (PDF)
- Opioid Resources for Prescribers
- Arkansas Medicaid Pharmacy Program Provider Memo — To access memos, follow the link, select Pharmacy from the menu bar, then select Memorandums from the drop-down options.
Preferred Blood Glucose Meters and Supplies
Please note that prior authorization may be required for certain products. The criteria document below is for reference only.
Traditional insulin pumps requiring tubing and cannula-type supplies will remain a medical benefit.
Submit prior authorization requests through the CoverMyMeds link above or send the prior authorization request form for prescription drugs to Pharmacy Services (see form linked above for details).
